Why is the study important?
One in 10 patients in an Australian hospital acquires an infection while in hospital. There are approximately 160,000 such infections acquired each year in Australian hospitals. These hospital- acquired infections represent just a subset of the total number healthcare associated infections (HAIs), which include all infections associated with receiving healthcare in all settings. The burden of HAIs is significant, with associated morbidity, mortality and, for those acquired in hospitals, increased length of stay.
However, there are limited randomised control trials exploring into the role of environmental cleaning to reduce HAIs. Prevention of infections through practical, implementable and translatable interventions is of critical importance in the era of antimicrobial resistance – not only to reduce the burden and impact for patients and health services now, but also to limit antimicrobial resistance and better prepare us for emerging infectious disease threats.
Contaminated patient environments provide a reservoir for pathogens to be transmitted to patients. Admission to a hospital room previously occupied by a patient infected and or colonised with a specific pathogen is a major risk factor for acquisition.
The proposed study builds on the REACH study findings, including important implementation strategies, and focuses on improving the cleaning of shared medical equipment as a key strategy in the reduction of HAIs.
Aim of the study
To demonstrate the effectiveness of improving the quality and frequency of cleaning shared medical equipment in reducing HAIs. A secondary objective is to evaluate the cost- effectiveness of the intervention.
What is the study?
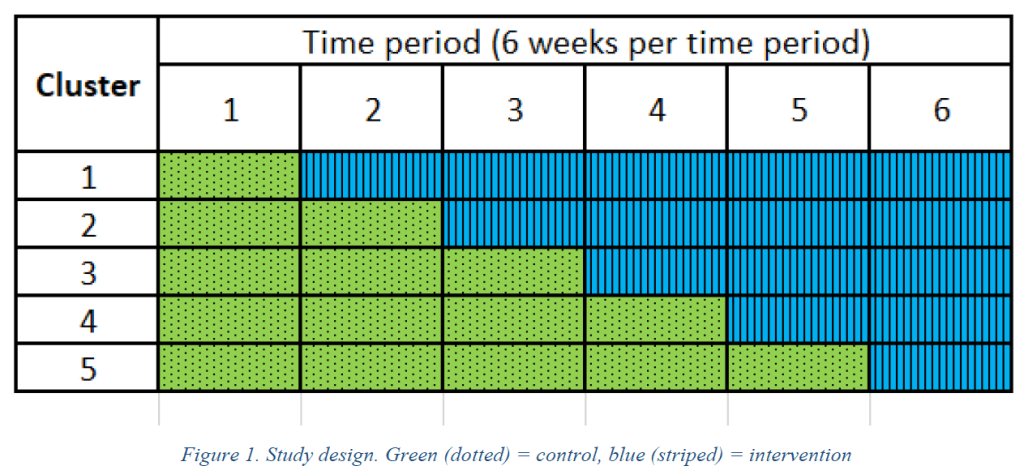
We are undertaking a stepped wedge randomised controlled study in 10 wards in one acute Australian hospital over 36 weeks.
The intervention
The intervention consists of
1) additional cleaning
2) education
3) audit and feedback on cleanliness to cleaning staff.
The additional cleaning involves three extra hours of cleaning each day per ward, and focusing on cleaning shared medical equipment such, but not limited to commodes, drip stands and computer on wheels.
Study outcomes
Primary outcome:
- The proportion of in-patients aged ≥18 years old with a HAI as measured by repeated HAI point prevalence studies (PPS).
Secondary outcomes:
- The thoroughness of cleaning as being the proportion of dots that were completely removed, as measured by the fluorescent markers gel and ultraviolet light system
- The cost-effectiveness of using the intervention